November 8, 2021
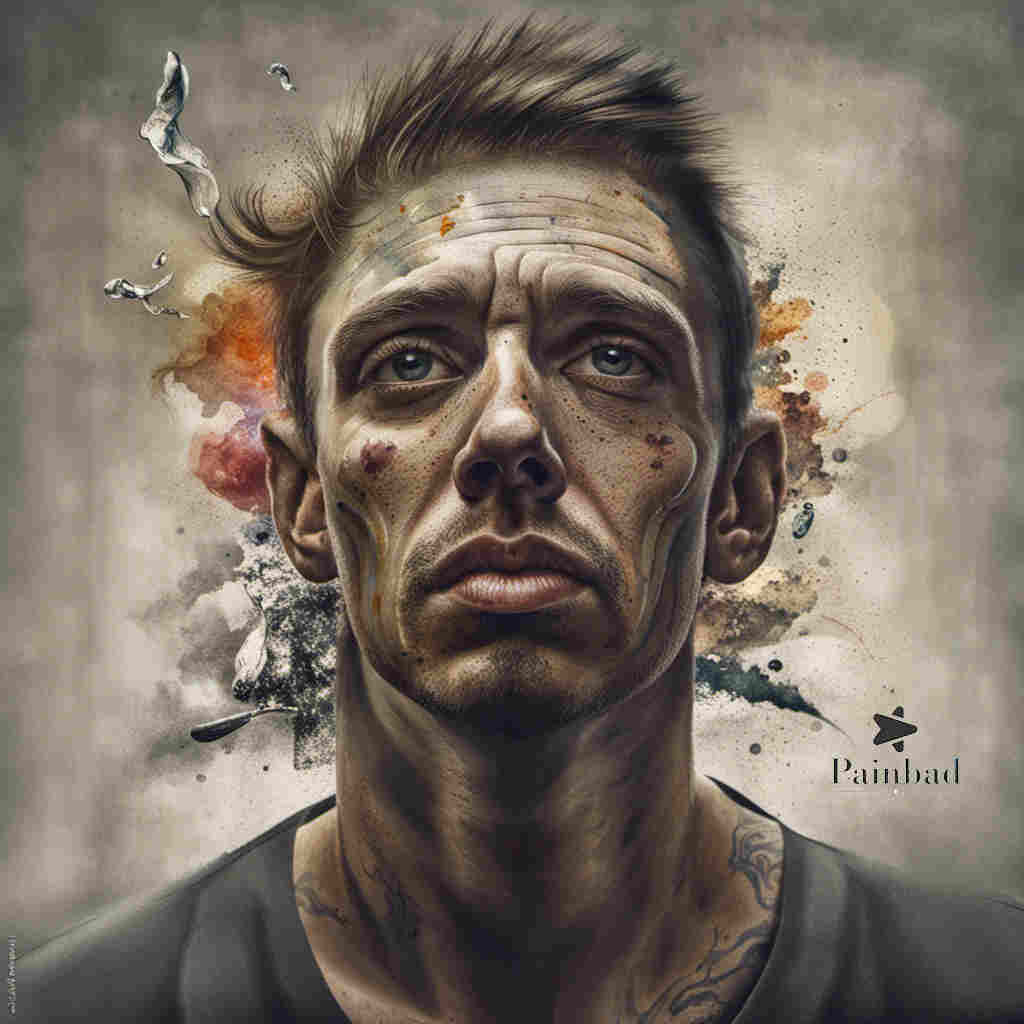
So, it’s great keeping a sort of pain diary. I suppose this public website is my pain diary.
The good thing is that you can really put things in perspective.
I know it was on October 5, 2021 that I first started feeling just a bit of the inflammatory pain concentrated in the gluteus…but also spreading out from there…my best guess is that this also in some way involved the psoas… I don’t know, though…I”m guessing…
Anyway, it was on October 7th that I had a check-up with the spine surgeon. There won’t be another one for a full year, but that’s another story. And, on the 7th, I told him my pain was a 2.5. And, that’s accurate.
And, that was the pain knocking on the door. Saying hello in a quiet voice. So, from the 7th on, the voice got louder. I got pretty ouchie. I didn’t take any steroids. I decided I just wanted to try and ride it out. So, I stopped taking classes. And, I started going easier at the workouts. In some cases, much easier.
And, starting yesterday…like a full month since that October 7, 2021 appointment…I finally felt the inflammation was down a lot…it’s hard to explain and talk about these things…but, that was the first day when I said, “Oh, man…it’s about gone. It’s still lingering around, but the wind got zapped from its sails…
It’s really hard to explain these things.
So, this inflammation is no joke. This isn’t the first time I’ve been through this…I’m telling you that inflammation can really linger around! For a long time!
I’m still going sort of easy because I’d rather not go through another month of that for a little bit…
And, I can kind of sense that it wouldn’t take much right now to flare it back up… I can just sort of sense that.
Here’s a bunch of research I did about inflammatory pain
Inflammatory Pain: Understanding the Mechanisms and Effects
Inflammatory pain is a type of pain that occurs as a result of the body’s immune response to tissue injury, infection, or other harmful stimuli. It is a complex physiological process involving various immune cells, chemical mediators, and signaling pathways. This type of pain serves as a protective mechanism to alert the body to potential threats and initiate the healing process. Understanding the mechanisms and effects of inflammatory pain is essential for effective pain management and treatment.
Mechanisms of Inflammatory Pain: Inflammatory pain arises from the activation of immune cells, such as mast cells, neutrophils, and macrophages, in response to tissue damage or infection. These cells release pro-inflammatory molecules, including cytokines (e.g., interleukins, tumor necrosis factor-alpha) and chemokines, which play a key role in sensitizing pain receptors, also known as nociceptors. Nociceptor sensitization leads to increased sensitivity to pain stimuli, causing heightened pain perception (Russo et al., 2007).
Additionally, inflammatory pain involves the activation of specialized receptors, such as Toll-like receptors (TLRs), which recognize danger signals released during tissue damage. TLR activation triggers intracellular signaling pathways that contribute to the release of pro-inflammatory molecules and further sensitization of nociceptors (Chen & Nuñez, 2010).
Effects and Characteristics: Inflammatory pain is often associated with distinct characteristics. It is typically described as a sharp, throbbing, or burning pain that is localized to the affected area. The pain is often exacerbated by movement or touch and can become chronic if the underlying inflammatory process persists. Inflammatory pain may also be accompanied by other symptoms like redness, swelling, and heat at the site of injury or infection.
One example of inflammatory pain is seen in conditions such as arthritis, where the inflammation of joints triggers pain signaling. Inflammatory pain can also be a component of conditions like infections, injuries, and autoimmune disorders. It serves as a crucial warning signal that prompts individuals to protect the affected area, avoid further damage, and seek appropriate medical care (Koltzenburg et al., 1999).
Management and Treatment: The management of inflammatory pain often involves addressing the underlying cause of inflammation while providing relief from pain symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to alleviate inflammatory pain by inhibiting the production of prostaglandins, which are responsible for promoting inflammation and sensitizing nociceptors. Corticosteroids may also be used to reduce inflammation and pain.
In some cases, specific medications targeting pain receptors or anti-inflammatory agents may be prescribed. Management strategies can also include physical therapy, rest, and lifestyle modifications.
Conclusion: Inflammatory pain is a complex process that plays a vital role in alerting the body to tissue damage and initiating the healing response. Understanding the mechanisms underlying inflammatory pain and its distinct characteristics is essential for effective pain management and improving the quality of life for individuals experiencing such pain.
References:
- Russo, R. E., Strong, J. A., & Schrader, J. A. (2007). Antinociceptive synergy between topical opioids and topical nonsteroidal anti-inflammatory drugs in the rat. European Journal of Pharmacology, 561(1-3), 103-107.
- Chen, G. Y., & Nuñez, G. (2010). Sterile inflammation: Sensing and reacting to damage. Nature Reviews Immunology, 10(12), 826-837.
- Koltzenburg, M., Wall, P. D., & McMahon, S. B. (1999). Does the right side know what the left is doing? Trends in Neurosciences, 22(3), 122-127.